HẸP ĐỘNG MẠCH NỘI SỌ DO XƠ VỮA – Nghiên cứu công bố trên tạp chí Lancet 2014
HẸP ĐỘNG MẠCH NỘI SỌ DO XƠ VỮA ĐỘNG MẠCH
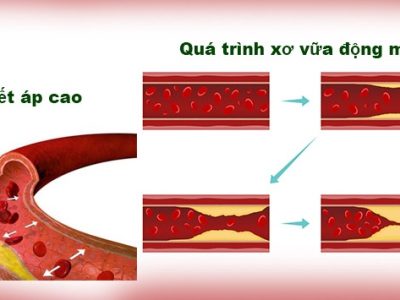
Hẹp động mạch nội sọ do xơ vữa là nguyên nhân đột quỵ của 5-10% người da trắng, 15-29% cơ thiếu máu não cục bộ hoặc đột quỵ của người da đen và là nguyên nhân gây đột quỵ khoảng 30-50% người Châu Á.
Yếu tố nguy cơ liên quan đến xơ vữa động mạch bao gồm tăng huyết áp, hút thuốc lá, đái tháo đường và rối loạn mỡ máu.
Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment
ICAS causes about 5–10% of strokes in white people, 15–29% of transient ischaemic attacks or strokes in black people, and up to 30–50% of strokes in Asian people.1–6 The frequency of ICAS as a cause of stroke also seems to be higher in northern India and Egypt than in white populations.7,8 Potential explanations for racial and ethnic differences in the prevalence of ICAS include genetic susceptibility of some racial and ethnic groups, and differences in lifestyle and risk factor profiles between races.2,9–12
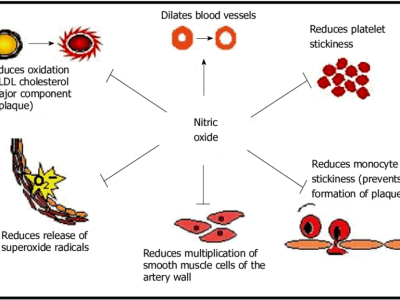
Traditional risk factors associated with ICAS include hypertension, smoking, diabetes mellitus, and hyperlipidaemia. 5,13–16 In the Warfarin Aspirin Symptomatic Intracranial Disease (WASID) trial, the most important modifiable risk factors for an increased risk of recurrent stroke and vascular events associated with ICAS were raised blood pressure and cholesterol concentrations.17 In the trial, which enrolled 569 patients with 50–99% symptomatic ICAS, the risk factors most strongly associated with recurrent ischaemic stroke and other major vascular events were mean systolic blood pressure greater than 140 mm Hg and mean cholesterol concentration greater than 5·20 mmol/L (200 mg/dl) during follow-up.1
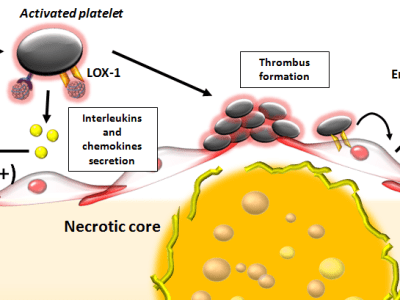
In a substudy of the Trial of cilOstazol in Symptomatic intracranial Stenosis 2 (TOSS-2) investigators examined potential lipoprotein predictors of ICAS progression in 230 patients with symptomatic stenosis of the middle cerebral artery and the basilar artery. Increased apolipoprotein B/A-I from baseline was associated with progression of stenosis on magnetic resonance angiography (MRA), whereas increased HDL concentrations were associated with stable stenosis.20 Other risk factors or biomarkers associated with an increased risk of recurrent stroke or progression of intracranial atherosclerosis include the metabolic syndrome,21,22 reduced adiponectin,23 increased lipoprotein-associated phospholipase A2,24 and increased C-reactive protein, E-selectin, plasminogen activator inhibitor-1, and lipoprotein (a).25
Some imaging characteristics, such as degree of stenosis and collateral circulation, affect risk of recurrent events and outcome in patients with ICAS. In the WASID trial, patients with at least 70% stenosis of a major intracranial artery had an increased risk of recurrent stroke in the territory of the stenosis compared with patients with 50–69% stenosis.26 However, the presence of robust collaterals in patients with greater than or equal to 70% stenosis mitigated the risk of recurrent stroke.27 In another study of 69 patients with symptomatic ICAS, Lau and colleagues28 showed that robust antegrade flow and good collaterals were protective against stroke.
The risk of recurrent stroke in patients presenting with transient ischaemic attacks or stroke also depends on how recently the ischaemic events occurred. In the WASID trial, patients whose qualifying event for the trial occurred 17 days or fewer before enrolment (the median time to enrolment in the trial) had a significantly higher risk of recurrent stroke during follow-up than did patients whose qualifying event for the trial occurred more than 17 days (up to 90 days) before enrolment.26