Cập nhật điều trị dự phòng đột quỵ do xơ vữa động mạch lớn nội sọ (2017- http://circres.ahajournals.org/)
Stroke Caused by Atherosclerosis of the Major Intracranial Arteries.
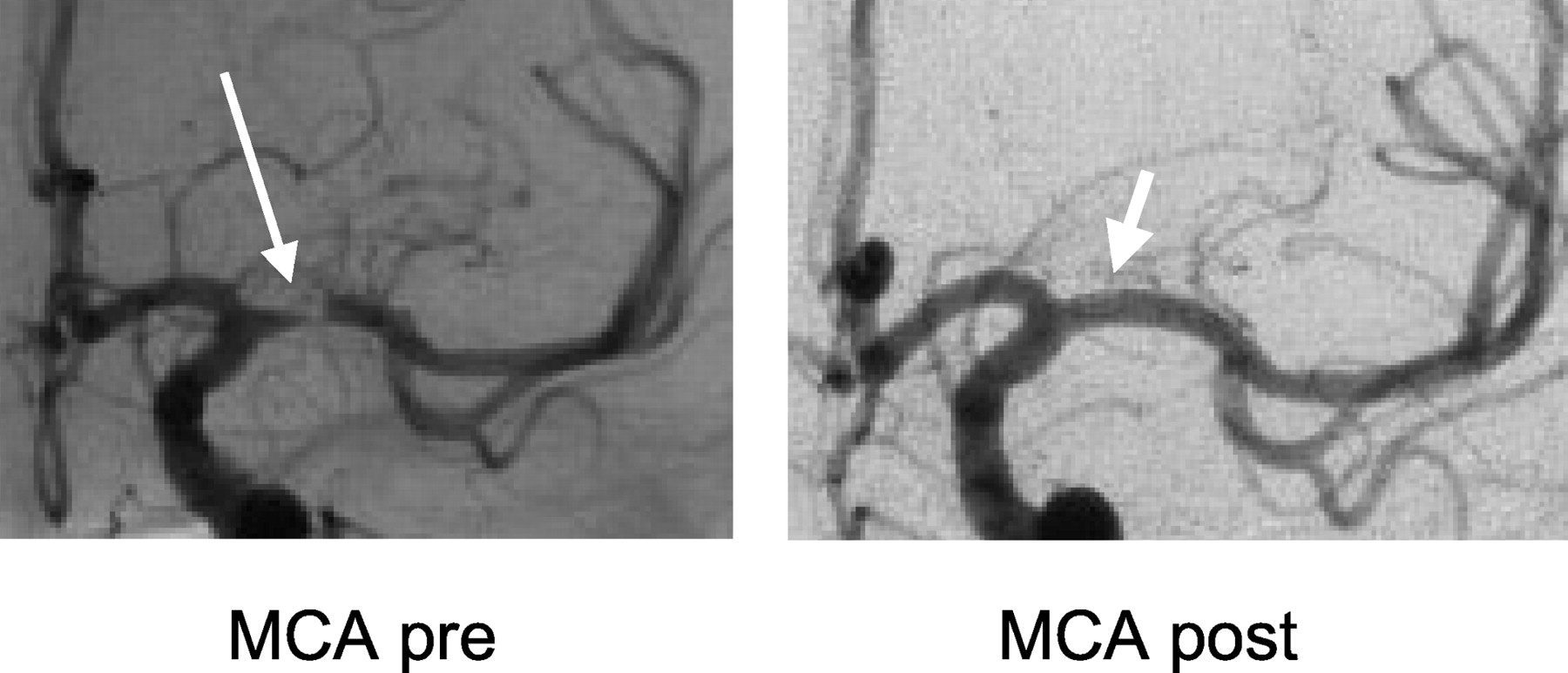
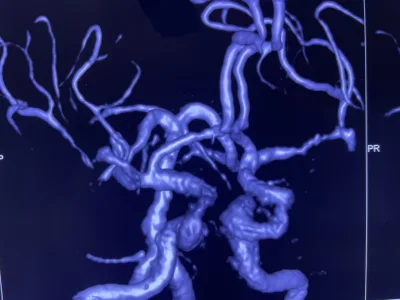
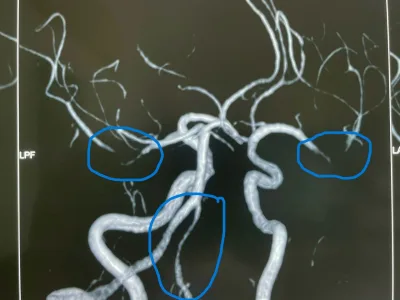
xĐặt stent động mạch não giữa trái đoạn M1
Summary
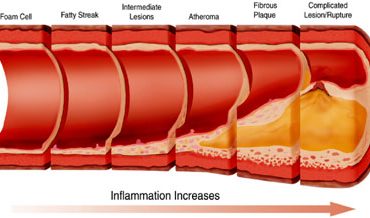
This excellent review identified references by searching PubMed for related studies published from 1955 to June 2016 using search terms intracranial stenosis and intracranial atherosclerosis. Reference sections of published randomized clinical trials and previously published reviews were searched for additional references. Included references number one hundred and thirty and contained within are the most relevant past and current articles on the subject. Twenty to 40 per 100000 people worldwide are estimated to suffer an intracranial atherosclerotic disease (ICAD) related ischemic event. Intracranial atherosclerotic disease is a highly prevalent cause of stroke that is associated with a high risk of recurrent stroke. The middle cerebral arteries are the most common site, followed by the basilar artery, the internal carotid arteries, and the intracranial vertebral arteries. It is more prevalent among blacks, Hispanics, and Asians compared to Caucasians. In terms of pathophysiology, the lack of an external elastic lamina along with impaired complement regulation, expression of ubiquitin proteasome conjugates and nuclear factor KB may explain the instability and susceptibility to inflammation in intracranial arteries. There are several possible mechanisms of ischemic stroke in the ICAD patients: artery to artery embolism, hypoperfusion and branch atheromatous disease and are seen as differing infarct patterns on neuroimaging. Computer tomographic angiography may be the most accurate of the non-invasive tests for defining a > 50% stenosis with sensitivity and specificity of 97% and 99.5% respectively compared to catheter angiography. Interesting, much like cervical carotid artery atherosclerotic disease, the risk of recurrent stroke increases with the severity of luminal stenosis such that those with a > 70% stenosis have an almost double risk of those with less stenosis. Poor collateral flow also increases the risk of stroke. The typical modifiable risk factors associated with atherosclerotic disease throughout the body are associated with intracranial atherosclerosis as well: diabetes mellitus, hypertension, metabolic syndrome, smoking, hyperlipidemia, and a sedentary lifestyle. Randomized clinical trials comparing aggressive management (dual antiplatelet treatment for 90 days followed by aspirin monotherapy and intensive management of vascular risk factors) with intracranial stenting plus aggressive medical management have shown medical management alone to be safer and more effective for preventing stroke. The most pertinent study regarding the use of intracranial stents is the NIH funded SAMMPRIS trial randomizing patients with a TIA or non-disabling stroke within the previous 30 days attributable to a 70-99% stenosis of a major intracranial artery to percutaneous transluminal angioplasty and stenting with the Wingspan stent plus aggressive medical management versus aggressive medical management alone. After treating 451 patients of the planned 764, enrollment was halted because of a higher rate of stroke or death in the stent group within 30 days of enrollment (14% vs 6%) of which 76% occurred within one day of the procedure. When followed for 1 and 2 years, the rate of stroke or death was similar between the two groups but the poor outcome at 30 days was never overcome. (Derdeyn CP, Chimowitz MI, Lynn MJ, et al. Stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis trial investigators. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet 2014;383:333-41). The high risk of recurrent stroke with best medical therapy, 12% and 15% at one and two years suggests there are subgroups of patients not protected by this treatment. Another study funded by industry to evaluate a different neurovascular stent resulted in the same fate. Open surgery consisting of an extracranial to intracranial bypass underwent a RCT in 1985 and ultimately reported a worse outcome in patients with middle cerebral artery stenosis. (The EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med 1985;313:1191-200). Future research needs to identify high-risks patients and target novel therapies to treat those so affected.
Conclusions
Aggressive medical management has become the standard of care for symptomatic patients with intracranial atherosclerotic disease. Nevertheless, there are subgroups of patients who are still at high risk of stroke despite being treated with aggressive medical management.